Obesity Challenges in older adults
Blog: January, 2026
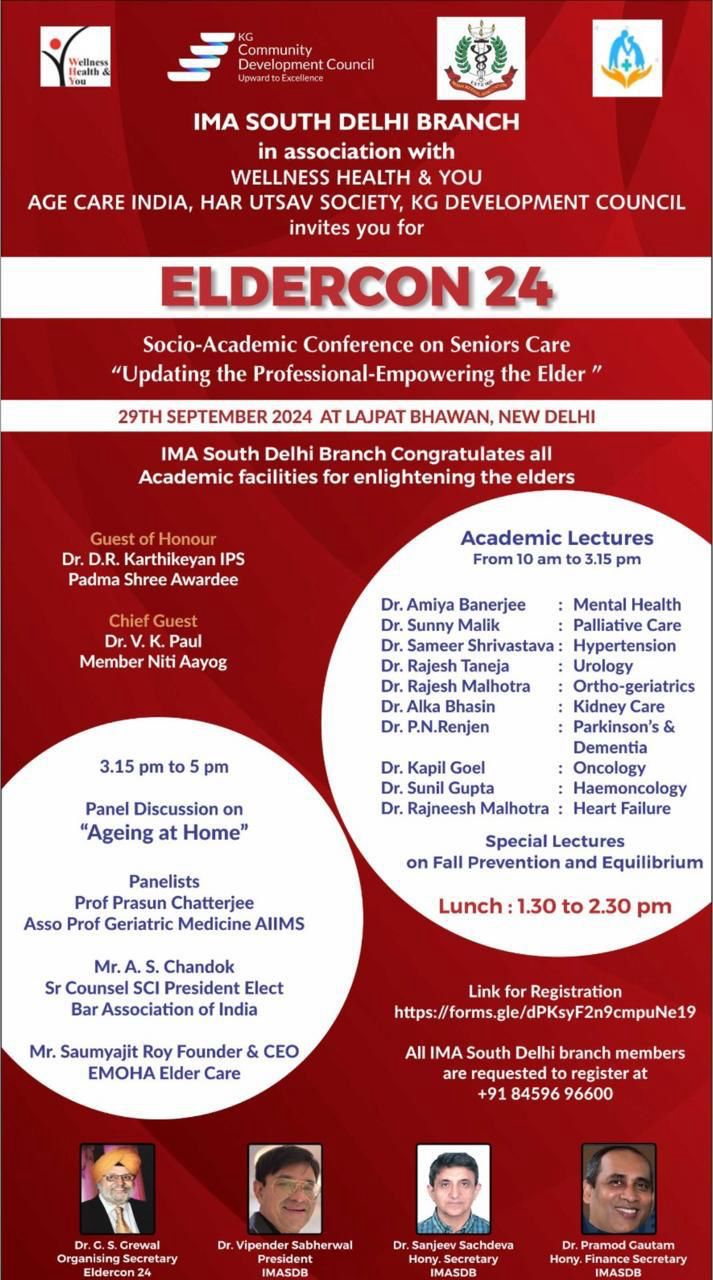
Source: http://www.aginghealthforum.com/
OBESITY CHALLENGES IN OLDER ADULTS
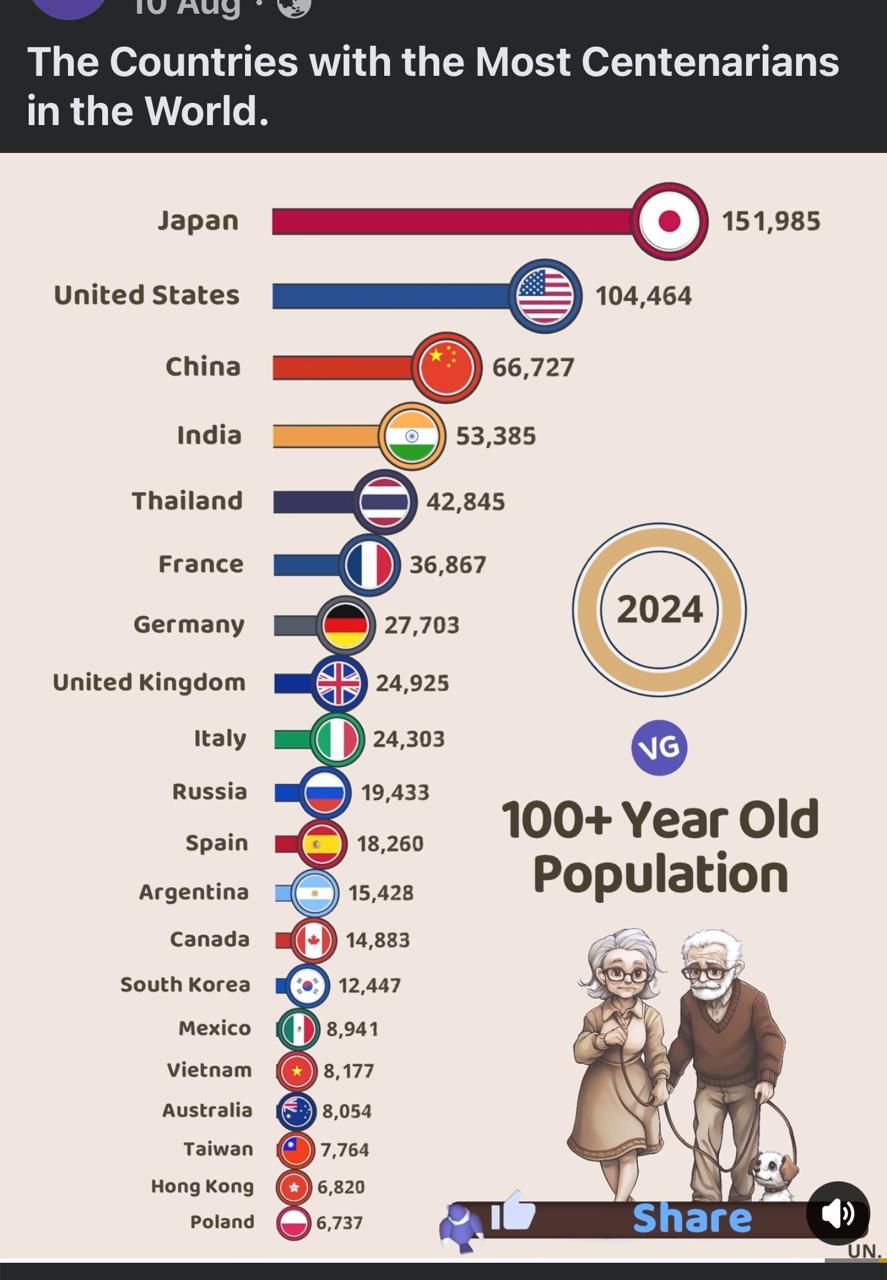
Obesity or fat accumulation in the body is highly prevalent across the world and is the mother of many lifestyle disorders. When it occurs in older adults, it presents unique challenges in detection and management.
Detection
As people age, they keep losing their fat free mass including muscles roughly at the rate of 3-8% per decade from the age 30 onwards. This age-related muscle loss or sarcopenia contributes to lighter body but is accompanied by increasing fat accumulation and its shifting from under the skin (subcutaneous tissue) to internal structures like liver, pancreas, heart etc. and the surrounding mesentery and omentum leading to visceral obesity which is even more risky for health. Body weight can remain normal, low or high in such a situation depending on the relative contribution of sarcopenia and obesity. The idiom “In sheep’s clothing perhaps, but still a wolf!” is probably apt to describe this situation where outward shape and appearance of the older adult may not suggest obesity (In sheep’s clothing) but yet this internal fat accumulation carries all the health risks of obesity (but still a wolf). We may as well call it as hidden or internal obesity. Obviously, body mass index {BMI), the conventional parameter to diagnose obesity (or fat accumulation) based on individual’s weight and height will fail in these circumstances. Moreover, old age is accompanied by some shortening of height and this may further compromise the ability of BMI to detect obesity in older adults. Other tools like measurement of waist circumference (WC), bioelectrical impedance analysis (BIA) and dual-energy X-ray absorptiometry (DEXA) will be more useful to measure obesity in such cases. Moreover, every older adult with obesity needs sarcopenia screening and if necessary further workup.
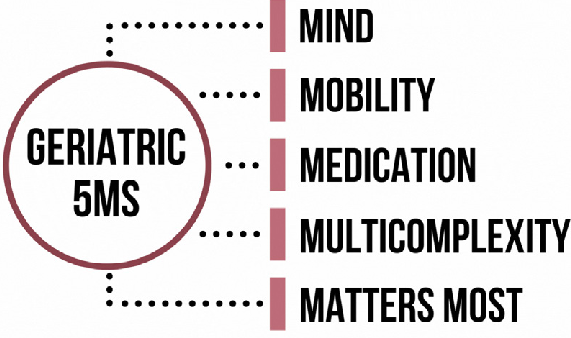
Older adults may harbour multimorbidity encompassing diabetes, hypertension, musculoskeletal diseases, cancer, chronic liver, kidney diseases etc. and many of these have their origin in obesity itself. Obesity in old age is also a risk factor for all the six age-related functional declines namely, cognition, psychology, mobility, vision, hearing, and nutrition compositely termed as intrinsic capacity by World Health Organization in their program of Integrated Care of the Older Persons (ICOPE). Hence these issues have to be specifically addressed while managing obesity in older adults by cognitive and psycho-social enhancement, multimodal exercises, caring for cataract, macular degeneration and retinopathy, hearing impairment if present and protein adequate dietary restrictions etc. Outlines of management of obesity in older adults are given below.
Management
Since older adults are a highly heterogenous lot in terms of their body composition of fat and fat free mass, coexisting morbidities, functional status and quality of life, individualising their obesity treatment is important. Secondly, in view of accelerated muscle loss in old age, caloric restriction employed for weight reduction should always be supplemented by adequate protein intake and prescribed strength training and other exercises to prevent further fat free and muscle loss.
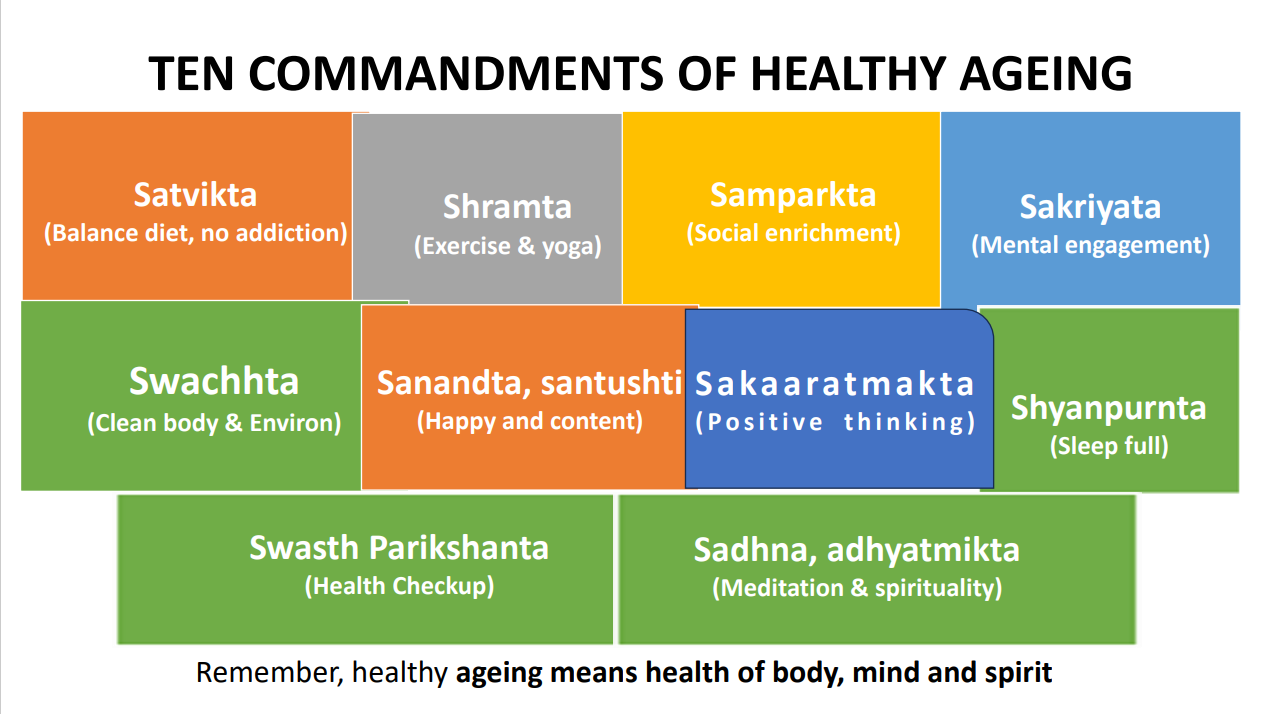
What to eat: A 500-700 calorie deficit diet with 1 to 1.2 gm of protein per Kg of actual body weight per day spread as 25-30 gm of proteins per meal is recommended. Supplements of powder or liquids for those who struggle to consume enough proteins. Adequate hydration.
When to eat: Traditional three main meals OK. Intermittent fasting like alternate day fasting or time restricted eating (e.g.16 hour fast and 8 hour feed) give the same benefit but to be careful for older adults for fear of possible fatigue, dizziness and hypoglycaemia during absence of meals. Various medicines they take also require food for absorption otherwise gastric irritation. Early to bed early to rise with light dinner well before sleep is better. The old adage “Breakfast like a king, Lunch like a prince and Dinner like a pauper” is questionable for older adults.
How to eat: Mindful eating and family and social dinning.
Exercises: prevent muscle and bone loss while caloric restriction or weight loss medicines are being pursued for obesity management. To be medically prescribed. Exercises to be multimodal-Aerobic (30-40 minutes a day for 5-7 days a week), Resistance (twice or thrice a week), Balancing. Stretching and Yoga. Those with limitations can do exercises in sitting position or pursue water based or internet guided but always medically supervised. Home based exercises with no or minimal equipment are also available for those who cannot go out due to bad weather or unfriendly roads and outdoor spaces.
Stress management: Depression, loneliness and sleeplessness are common in old age and can lead to food cravings, emotional eating, attenuation of satiety and non-compliance to life style practices and medications. Socializing, Yoga, Pranayama and Meditation for busting the stress. Sleep hygiene.
Cognitive enhancement: by Self-Brain Challenging Exercises, Recollection Exercises and Stimulation through Senses Exercises.
Pharmacological Interventions: comprise pruning or replacing weight promoting medications under medical advice which older adults may be taking inadvertently and use of modern day anti-obesity medications like GLP-Receptor Agonists again under Medical advice

_20240725123207.jpg)